Pancreatic Cancer Risk Calculator
Assess Your Risk Factors
Based on research from the article. This is not medical advice.
Risk Assessment Results
Important: Most pancreatic cancer cases are diagnosed late (80% at stage III/IV). Early symptoms include unexplained weight loss, jaundice, and new-onset diabetes after age 50. Learn more about symptoms.
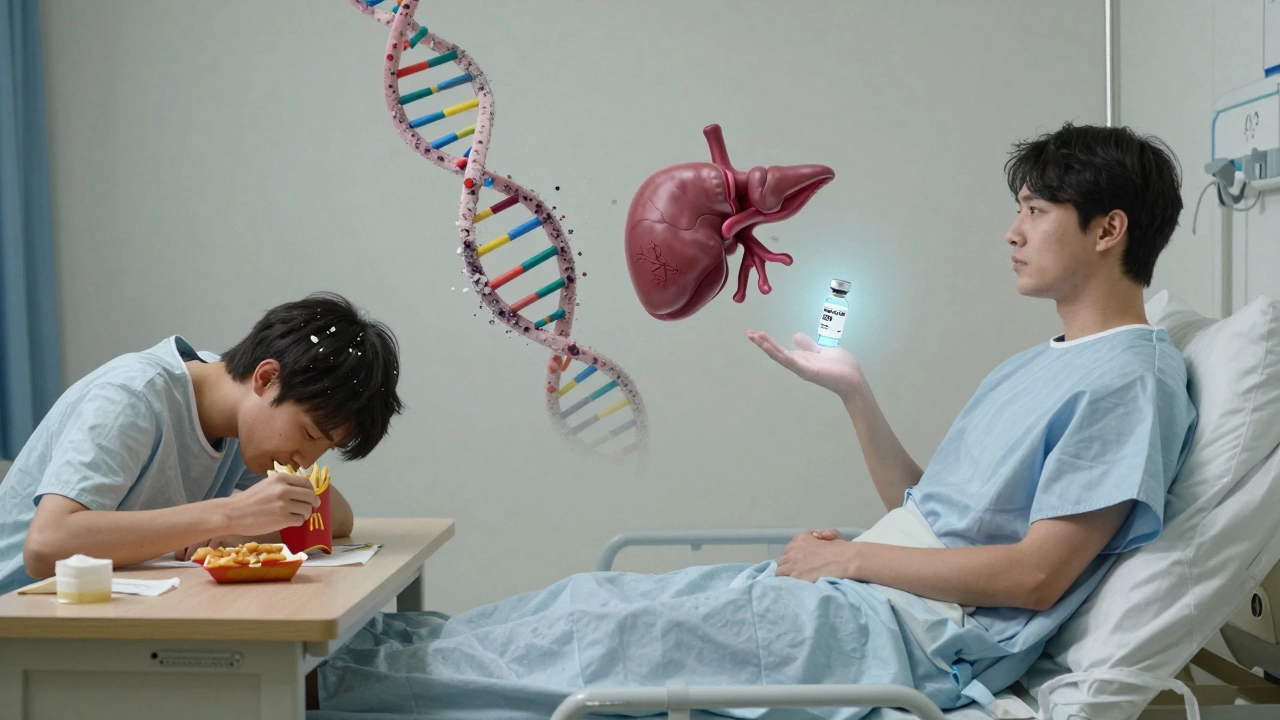
When people hear the word cancer, their minds often go to one specific type - the one that doesn’t just spread, but slips through fingers before anyone even knows it’s there. It’s not the most common. It’s not the most talked about in ads or walks for awareness. But it’s the one that terrifies doctors, survivors, and families alike. That cancer is pancreatic cancer.
Why Pancreatic Cancer Feels Like a Silent Killer
Pancreatic cancer doesn’t shout. It doesn’t cause a lump you can feel. It doesn’t make you cough or bleed. By the time symptoms show up - back pain, jaundice, unexplained weight loss, new-onset diabetes - the cancer has often already spread beyond the pancreas. About 80% of cases are diagnosed at stage III or IV. That means the tumor has either invaded nearby organs or traveled to the liver, lungs, or peritoneum.
The pancreas sits deep in the abdomen, tucked behind the stomach. It’s not an organ you notice unless something goes terribly wrong. And when it does, the body rarely gives early warning signs. There’s no routine screening test like a mammogram or colonoscopy. No blood test you can take at your annual checkup that reliably catches it early.
Survival Rates That Break Your Heart
The five-year survival rate for pancreatic cancer is around 12%. For localized cases - where it hasn’t spread - it’s about 44%. But only 10% of patients are diagnosed at that stage. Once it spreads to distant organs, survival drops to 3%. Those numbers haven’t changed much in 30 years. For comparison, breast cancer has a 91% five-year survival rate. Prostate cancer? Nearly 100%. Even lung cancer, which used to be a death sentence, now has targeted therapies and immunotherapies pushing survival rates higher.
Why hasn’t pancreatic cancer kept up? Because it’s biologically stubborn. It’s surrounded by dense tissue called stroma, which acts like a shield. Chemotherapy drugs struggle to reach the tumor. The cancer cells mutate quickly. They adapt to treatment before doctors even finish the first round.
Who’s at Risk - And Why It’s Not Just About Smoking
Most people assume smoking is the biggest cause. And yes, smokers are twice as likely to get pancreatic cancer. But many patients never smoked. Others never drank. Some were active, ate well, and had no family history.
Here’s what actually increases risk:
- Chronic pancreatitis - long-term inflammation of the pancreas
- Hereditary syndromes like BRCA1/BRCA2 mutations (same genes linked to breast cancer)
- Long-standing type 2 diabetes, especially if diagnosed after age 50
- Obesity - especially carrying excess weight around the abdomen
- Age - most cases occur after 65
- Family history - having two or more close relatives with pancreatic cancer
There’s also a scary trend: more cases in people under 50. In the U.S., incidence in younger adults has risen by over 1% per year since the 1990s. No one knows why.

What Does Treatment Look Like Today?
There’s no magic bullet. Surgery - the Whipple procedure - is the only chance for cure. But only 15% to 20% of patients are candidates. The tumor has to be contained, not touching major blood vessels. Even then, recurrence rates are high.
Chemotherapy is the mainstay. FOLFIRINOX and gemcitabine with nab-paclitaxel are the two most common regimens. They extend life by months, sometimes over a year. But they come with brutal side effects: nausea, nerve damage, extreme fatigue, low blood counts.
Immunotherapy? It barely works here. Unlike melanoma or lung cancer, pancreatic tumors don’t respond well to checkpoint inhibitors. The stroma blocks immune cells from even reaching the cancer.
But there’s hope. Clinical trials are testing new approaches:
- Personalized vaccines made from a patient’s own tumor cells
- Drugs that break down the stroma barrier
- Targeted therapies for rare mutations like KRAS G12C
- Early detection blood tests looking for tumor DNA fragments
One trial at the Royal Marsden Hospital in London showed a 50% reduction in recurrence risk for patients who received a personalized mRNA vaccine after surgery. It’s not a cure. But it’s a step.
The Emotional Weight of a Diagnosis
It’s not just the numbers. It’s the speed. People go from feeling fine to being told they have months to live. No time to plan. No time to say goodbye properly. No time for second opinions. Families scramble. Insurance battles begin. Children grow up without a parent who never got to see them graduate.
And there’s a stigma. Because it’s linked to smoking and drinking, some assume the patient brought it on themselves. That’s cruel and wrong. Many patients had no risk factors. They were healthy, active, and unaware.
What You Can Do - Even If You’re Not at Risk
You can’t prevent all cancers. But you can reduce your risk:
- Don’t smoke. Period.
- Maintain a healthy weight. Even losing 5-10% of body weight lowers risk.
- Move daily. Walking 30 minutes a day reduces risk by 15%.
- Watch your sugar. High sugar intake and processed carbs increase insulin resistance - a known risk factor.
- Know your family history. If two relatives had pancreatic cancer, talk to a genetic counselor.
- Pay attention to new symptoms. Unexplained weight loss, dark urine, yellow eyes, or persistent abdominal pain after age 50? Get checked. Don’t wait.
There’s no vaccine. No magic pill. But awareness saves lives. Early detection - even if it’s just one extra person catching it before it spreads - changes everything.
Why This Cancer Still Holds So Much Fear
Pancreatic cancer scares us because it’s unpredictable. It doesn’t care if you’re fit, young, or careful. It doesn’t announce itself. And when it does, it’s often too late.
But fear doesn’t have to mean helplessness. Understanding the risks. Knowing the symptoms. Pushing for answers when something feels off. That’s how we fight back.
Every new trial. Every blood test in development. Every doctor who listens when a patient says, ‘Something’s not right.’ - that’s where hope lives.
Is pancreatic cancer the deadliest cancer?
Yes, by survival rate. While lung cancer kills more people each year due to higher incidence, pancreatic cancer has the lowest five-year survival rate among major cancers - around 12%. That’s because it’s rarely caught early and resists most treatments.
Can pancreatic cancer be cured?
It can be cured only if caught very early - before it spreads - and if the tumor can be surgically removed. That happens in only about 15% of cases. Even then, recurrence is common. For most, the goal is to extend life and improve quality, not to cure.
What are the first signs of pancreatic cancer?
Early signs are vague: unexplained weight loss, loss of appetite, new-onset diabetes after age 50, jaundice (yellow skin or eyes), dark urine, light-colored stools, and persistent pain in the upper abdomen that radiates to the back. These symptoms often appear only after the cancer has grown or spread.
Is pancreatic cancer hereditary?
Yes, in about 10% of cases. Inherited mutations in genes like BRCA1, BRCA2, PALB2, Lynch syndrome genes, or familial pancreatic cancer syndromes increase risk. If two or more close relatives had pancreatic cancer, genetic testing may be recommended.
Why is pancreatic cancer so hard to treat?
It’s surrounded by a thick layer of tissue called stroma that blocks drugs and immune cells. The cancer cells mutate rapidly, making them resistant to chemotherapy and immunotherapy. There’s also no reliable early detection test, so most cases are diagnosed too late for surgery.





