Diabetes Medication Selector
Find which diabetes medications may be most appropriate for your unique health profile. This tool provides evidence-based recommendations based on the article's key principles. Note: This is not medical advice. Always consult your healthcare provider.
Recommended Medications
Recommendations are based on evidence from the article. This tool does not replace professional medical advice.
There’s no single "strongest" medicine for diabetes that works for everyone. The idea that one drug can crush high blood sugar for all patients is a myth. Diabetes isn’t just about blood sugar levels-it’s about your body’s unique response to insulin, your weight, your heart health, your kidneys, and even your lifestyle. What works like magic for one person might do nothing-or even cause problems-for another.
Why There’s No Universal "Strongest" Diabetes Drug
Diabetes isn’t one disease. Type 1 means your body doesn’t make insulin at all. Type 2 means your body resists insulin or doesn’t make enough. Then there’s gestational diabetes, LADA, and other rare forms. Each needs a different approach.
Some people think insulin is the "strongest" because it directly lowers blood sugar. But insulin isn’t always the first choice-even for Type 2. Why? Because it can cause weight gain and low blood sugar. For many, starting with something gentler, like metformin, makes more sense. It doesn’t cause weight gain. It doesn’t cause hypoglycemia on its own. And it’s been used safely for over 60 years.
Other drugs, like SGLT2 inhibitors and GLP-1 receptor agonists, don’t just lower sugar. They protect your heart and kidneys. In some cases, they help you lose weight. That’s not just treatment-it’s disease modification.
Metformin: The Foundation, Not the Strongest
Metformin is the most prescribed diabetes drug in the world. It’s cheap. It’s safe. And for most people with Type 2 diabetes, it’s the first step.
How it works: Metformin reduces how much sugar your liver releases and makes your muscles more sensitive to insulin. It doesn’t force your body to make more insulin. That’s why it rarely causes low blood sugar.
Side effects? Upset stomach, bloating, diarrhea. Most people get used to it after a few weeks. Taking it with food helps. Extended-release versions are easier on the stomach.
But here’s the truth: metformin alone often isn’t enough long-term. About half of people with Type 2 diabetes will need another drug within five years. That doesn’t mean metformin failed. It means diabetes is progressive.
GLP-1 Agonists: The New Power Players
If you’re looking for the most powerful single-class drugs today, GLP-1 receptor agonists are it. Drugs like semaglutide (Wegovy, Ozempic), liraglutide (Victoza), and dulaglutide (Trulicity) don’t just lower blood sugar-they change how your body handles food.
They slow digestion, reduce appetite, and help your pancreas release insulin only when needed. That means fewer spikes and crashes. And because they reduce hunger, most people lose 10-15% of their body weight. That’s not a side effect-it’s part of the treatment.
A 2023 study in The New England Journal of Medicine showed that semaglutide reduced the risk of heart attack, stroke, or death by 20% in people with Type 2 diabetes and heart disease. That’s bigger than any other diabetes drug has ever done.
But they’re injectables. They cost more. And they can cause nausea, especially at first. Not everyone tolerates them. But for those who do, they’re often the most effective single therapy available.
Insulin: When You Need the Heavy Lifter
Insulin is the original and most direct way to lower blood sugar. It’s essential for Type 1 diabetes. Many people with Type 2 eventually need it too.
There are different kinds: long-acting (like glargine or degludec) for baseline control, and fast-acting (like lispro or aspart) for meals. Some people use a combination.
Insulin is powerful-but it’s not precise. Too much and you risk low blood sugar. Too little and sugar stays high. It requires constant monitoring and careful dosing. That’s why many doctors delay starting insulin until other options are tried.
But if your A1C is above 9% and you’re losing weight, feeling tired, or urinating constantly, insulin might be the only thing that brings your numbers down fast enough to protect your organs.
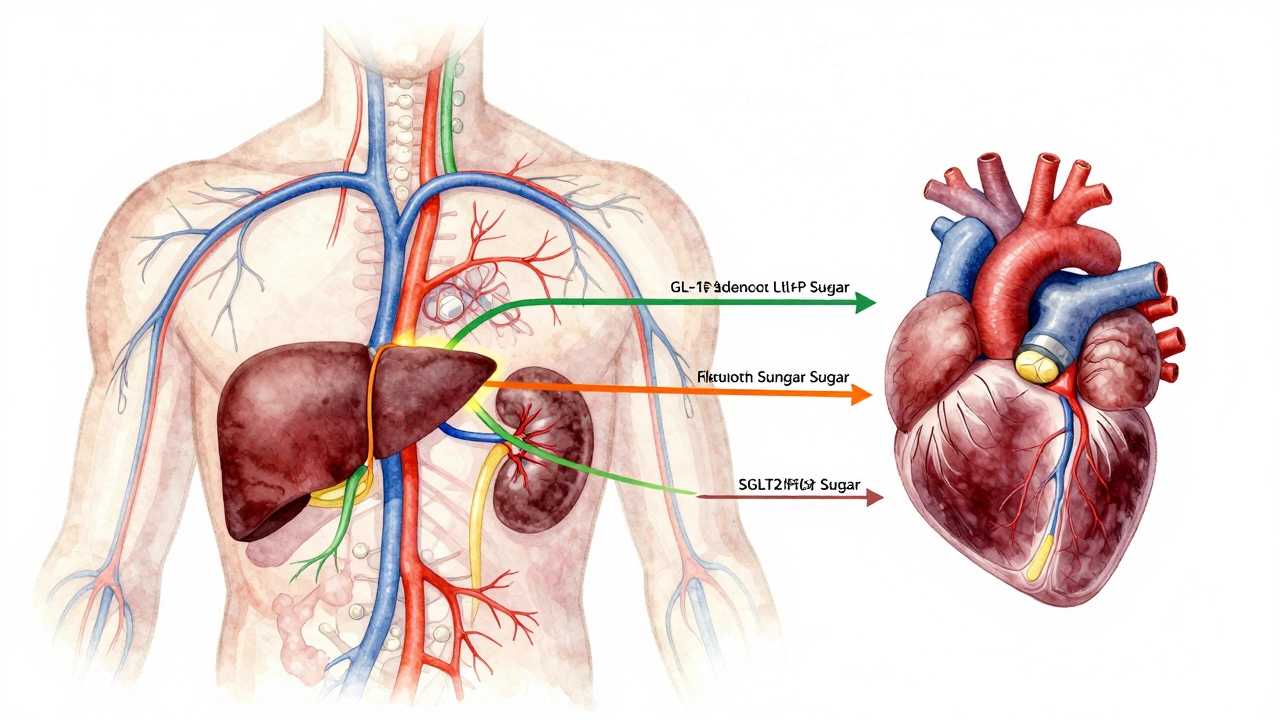
SGLT2 Inhibitors: Strong Because They Do More Than Lower Sugar
Drugs like empagliflozin (Jardiance), dapagliflozin (Farxiga), and canagliflozin (Invokana) work by making your kidneys dump sugar out through urine. Sounds strange, right? But it’s brilliant.
They lower A1C by 0.5-1%. They help you lose weight. They lower blood pressure. And they cut your risk of heart failure hospitalization by up to 30%.
Studies show people taking empagliflozin lived longer and had fewer kidney problems. In fact, the FDA approved it not just for diabetes, but for heart failure and chronic kidney disease-even in people without diabetes.
Downsides? You might get yeast infections or urinary tract infections. You need to drink more water. Rarely, they can cause a dangerous condition called euglycemic diabetic ketoacidosis. But for most, the benefits far outweigh the risks.
Combination Therapy: The Real Secret to Success
Doctors rarely rely on just one drug anymore. The strongest approach is often combining two or three with different mechanisms.
For example: metformin + a GLP-1 agonist + an SGLT2 inhibitor. That’s a triple punch. One reduces liver sugar, one reduces appetite and boosts insulin, one flushes out sugar through urine. Together, they can drop A1C by 2-3 points-more than any single drug.
There are even combo pills now: metformin + empagliflozin, or metformin + sitagliptin. Fewer pills. Fewer decisions. Better adherence.
And the results? People on combination therapy are less likely to need insulin later. Their hearts and kidneys stay healthier. They lose weight. They feel better.
What Doesn’t Work as Well (And Why)
Some older drugs are still around-but they’re fading out.
Sulfonylureas (like glimepiride or glyburide) force your pancreas to make more insulin. They lower sugar, yes. But they cause weight gain and low blood sugar. They don’t protect your heart. Many guidelines now recommend avoiding them as first-line.
Thiazolidinediones (like pioglitazone) improve insulin sensitivity but cause fluid retention, weight gain, and can worsen heart failure. They’re rarely used now.
And don’t fall for the myth that "natural" supplements like cinnamon, berberine, or bitter melon can replace medication. Some studies show small, temporary effects. None have proven they prevent complications like heart disease, kidney failure, or blindness.

Choosing the Right Medicine for You
Your doctor doesn’t pick a drug because it’s "strongest." They pick based on:
- Your A1C level and how high your blood sugar is
- Whether you have heart disease, kidney disease, or obesity
- Your risk of low blood sugar
- Your budget and insurance coverage
- Whether you’re willing to take injections
- Your lifestyle and daily routine
For someone with obesity and heart disease? A GLP-1 agonist might be the best choice.
For someone with kidney disease? An SGLT2 inhibitor could be lifesaving.
For someone just diagnosed with mild Type 2? Metformin is still the gold standard.
There’s no one-size-fits-all. That’s why you need a doctor who listens-not just one who prescribes.
What Happens If Medication Isn’t Enough?
Medication isn’t the whole story. Even the strongest drug won’t fix a diet full of sugar, a sedentary life, or chronic stress.
Weight loss of just 5-10% can put Type 2 diabetes into remission for many. That’s not a miracle. It’s science. The liver stops flooding the body with sugar. The pancreas gets a break. Insulin sensitivity improves.
Exercise? It makes your muscles use glucose without needing insulin. Just 30 minutes a day, five days a week, can lower A1C by 0.5-1%.
And sleep? Poor sleep raises cortisol, which raises blood sugar. Stress management? It lowers inflammation, which drives insulin resistance.
Medication is a tool. Lifestyle is the foundation.
Final Thought: Strength Isn’t About Potency-It’s About Results
The strongest medicine for diabetes isn’t the one with the highest dose or the most dramatic name. It’s the one that keeps your A1C below 7%, protects your heart, keeps your kidneys working, helps you live longer, and lets you feel like yourself again.
For some, that’s metformin. For others, it’s semaglutide. For many, it’s a mix. And for all of them, it’s paired with real, sustainable changes in how they eat, move, and live.
There’s no magic bullet. But there are smart, science-backed options. The key is working with your healthcare team to find the right combination-for your body, your life, and your future.
Is insulin the strongest diabetes medicine?
Insulin is the most direct way to lower blood sugar, but it’s not always the "strongest" in terms of overall benefit. It can cause weight gain and low blood sugar. Newer drugs like GLP-1 agonists and SGLT2 inhibitors often do more-they protect the heart and kidneys, help with weight loss, and reduce long-term risks. Insulin is essential for Type 1 diabetes and advanced Type 2, but it’s not the first choice for everyone.
Can GLP-1 agonists cure diabetes?
GLP-1 agonists like semaglutide don’t cure diabetes, but they can lead to remission in some people with Type 2 diabetes-especially when combined with weight loss. Remission means blood sugar stays normal without medication. This happens when fat around the liver and pancreas drops, allowing those organs to work better. It’s not permanent for everyone, but it’s possible.
Are there any diabetes medicines that help you lose weight?
Yes. GLP-1 agonists (like Ozempic, Wegovy, Trulicity) and SGLT2 inhibitors (like Farxiga, Jardiance) often cause weight loss. GLP-1 drugs reduce appetite and slow digestion, leading to 10-15% weight loss in many users. SGLT2 inhibitors cause you to lose sugar through urine, which also burns calories. Weight loss isn’t just a side effect-it’s a key part of how these drugs improve long-term outcomes.
Why do doctors start with metformin instead of stronger drugs?
Metformin is safe, cheap, doesn’t cause low blood sugar or weight gain, and has been proven to reduce complications over decades. It’s the best first step for most people. Stronger drugs like GLP-1 agonists are more expensive and may have side effects like nausea. Doctors use them when metformin alone isn’t enough or when extra benefits (like heart protection or weight loss) are needed.
Can I stop taking diabetes medication if I lose weight?
Some people with Type 2 diabetes can reduce or stop medication after losing 5-10% of their body weight, especially if they improve their diet and exercise. But this isn’t guaranteed. Even if blood sugar normalizes, the underlying risk remains. Stopping medication without medical supervision can be dangerous. Always work with your doctor to adjust treatment safely.





