Pancreatic Cancer Survival Rate Calculator
How Your Diagnosis and Treatment Affect Survival
Pancreatic cancer survival rates vary significantly based on stage at diagnosis and treatment options. This calculator estimates 5-year survival chances using current medical data.
Your Situation
Survival Estimate
5-year survival rate
Based on current medical data, your estimated 5-year survival rate is calculated from:
- Stage at diagnosis
- Treatment options selected
When someone hears the word cancer, their mind often races to the worst-case scenario. But not all cancers are the same. Some respond well to treatment. Others barely budge, no matter how hard doctors push. Among them, one stands out as the most stubborn: pancreatic cancer.
Pancreatic Cancer Is the Hardest to Cure
Pancreatic cancer doesn’t just spread fast-it hides. It grows silently inside the abdomen, often without symptoms until it’s already advanced. By the time most people are diagnosed, the cancer has either spread to nearby organs or invaded major blood vessels. That’s why only about 12% of patients survive five years after diagnosis. For some subtypes, the number drops below 5%.
Compare that to breast cancer, where survival rates have climbed to over 90% for early-stage cases, or even thyroid cancer, where most patients live normal lifespans after treatment. Pancreatic cancer doesn’t play by the same rules. It doesn’t respond well to chemotherapy. It doesn’t shrink easily with radiation. And surgery? Only about 15% to 20% of patients are even eligible.
Why Is It So Hard to Treat?
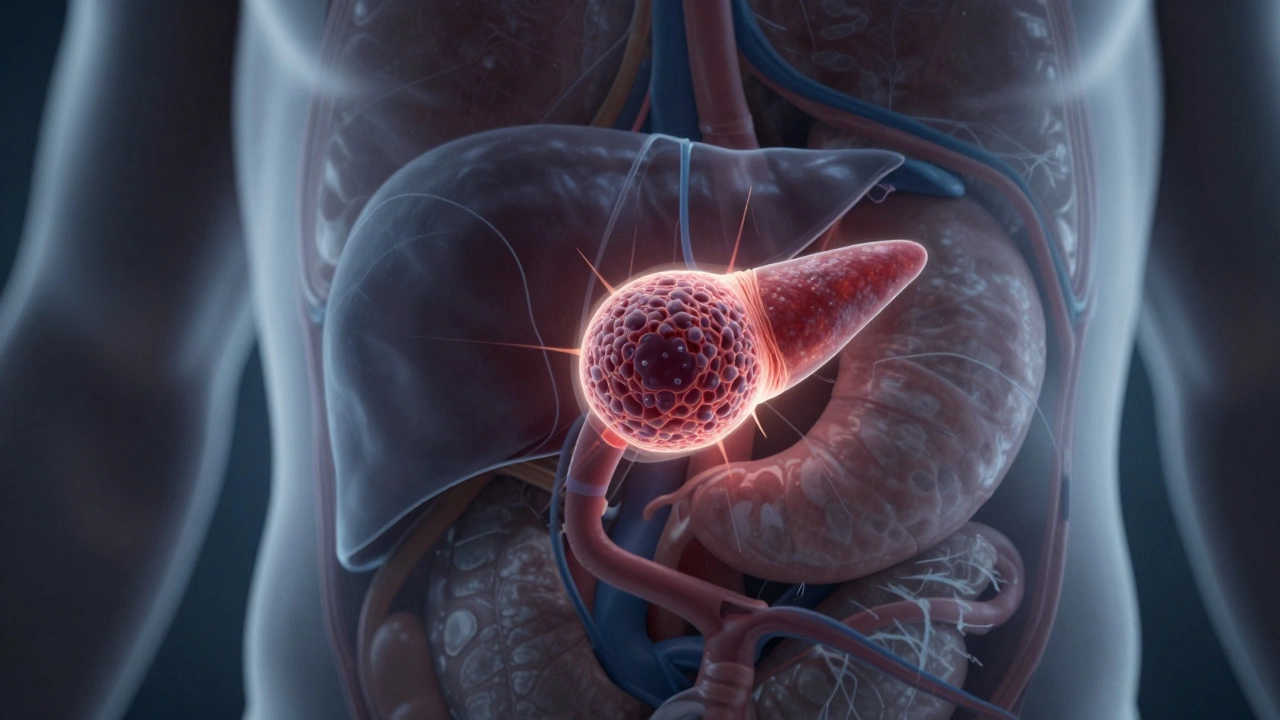
The pancreas sits deep in the body, wrapped by the liver, stomach, and major arteries. Tumors here don’t show up on routine scans. There’s no blood test that catches it early. Even when doctors suspect it, confirming the diagnosis often requires invasive procedures like endoscopic ultrasounds or biopsies that carry their own risks.
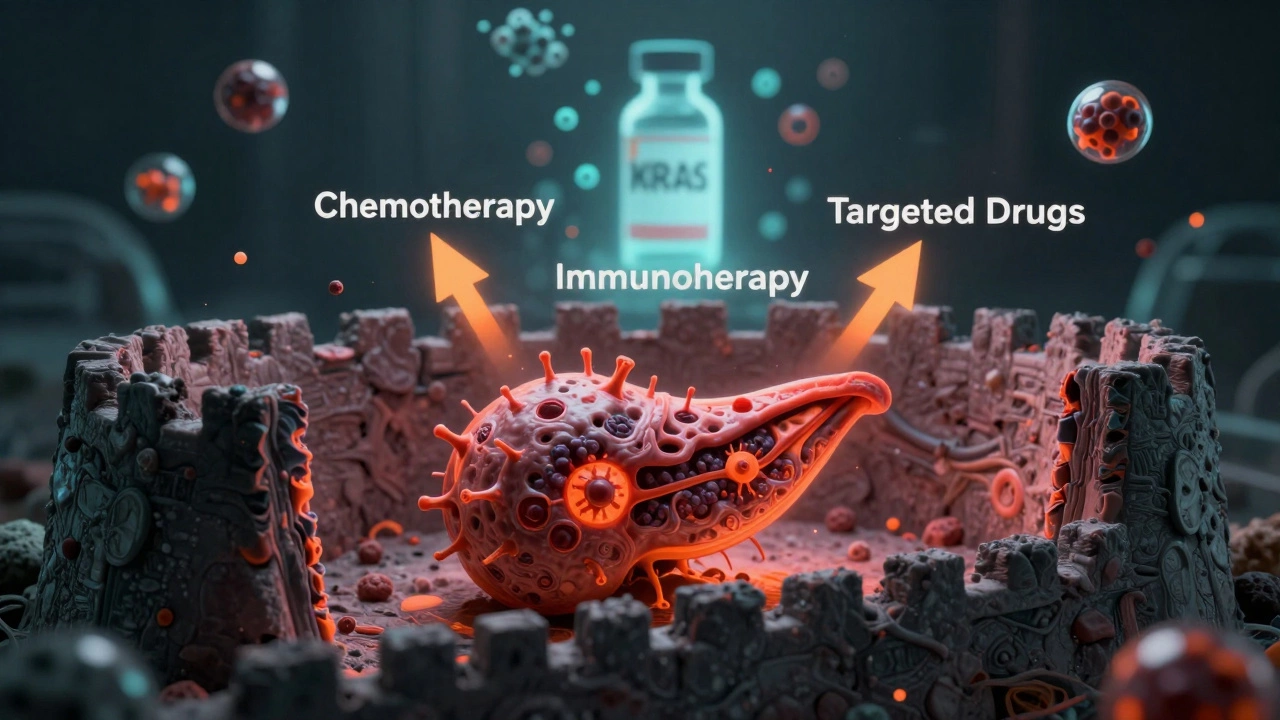
Once the cancer takes hold, it builds a protective shield. The tumor creates a dense wall of scar-like tissue called stroma. This stroma blocks drugs from reaching cancer cells. It also suppresses the immune system’s ability to attack. Think of it like a fortress with moats, walls, and guards that shut out every kind of weapon-chemotherapy, immunotherapy, even targeted drugs.
Unlike lung or skin cancers, which often have clear genetic triggers that drugs can target, pancreatic cancer is genetically messy. Tumors carry dozens of mutations at once, and they change rapidly. A drug that works one month might be useless by the next. This constant evolution makes personalized treatment a moving target.
Early Detection Is Almost Impossible
There’s no screening test for pancreatic cancer like there is for colon or cervical cancer. Mammograms, Pap smears, colonoscopies-those catch cancers early. Nothing like that exists for the pancreas. By the time someone feels pain in their upper belly, loses weight without trying, or develops jaundice, the cancer is usually stage III or IV.
Some high-risk groups-people with inherited gene mutations like BRCA1, Lynch syndrome, or chronic pancreatitis-are monitored more closely. But even then, catching it early is rare. A 2023 study tracking 1,200 high-risk individuals found that only 1 in 7 early-stage tumors were detected before they spread.
What About New Treatments?
There’s hope-but it’s slow. Researchers are testing new ways to break through the stroma. One approach uses drugs that target the fibrous tissue around tumors, making them more vulnerable to chemotherapy. Another combines immunotherapy with radiation to wake up the immune system inside the tumor.
Some clinical trials are showing promise with mRNA vaccines tailored to a patient’s specific tumor mutations. These vaccines train the body to recognize and attack cancer cells like a custom-made missile. Early results in small groups show longer survival times, but these are still experimental.
There’s also a new class of drugs called KRAS inhibitors. For decades, KRAS mutations-found in over 90% of pancreatic cancers-were considered “undruggable.” But in 2021, sotorasib became the first drug to block a specific KRAS mutation. It’s not a cure, but for some patients, it shrinks tumors and buys extra months. Newer versions are now being tested in combination therapies.
Other Tough Cancers-But None as Bad
Pancreatic cancer isn’t the only hard one. Glioblastoma, a brain cancer, also has a grim prognosis. Most patients live less than 15 months after diagnosis. Lung cancer that’s spread to other organs is another killer. But even these cancers have better options than pancreatic cancer.
Glioblastoma patients can sometimes get surgery, radiation, and the drug temozolomide. Lung cancer patients often respond to immunotherapy or targeted therapies if they have EGFR or ALK mutations. Pancreatic cancer patients rarely have those lucky mutations. Only 5% to 10% have BRCA mutations that make them eligible for PARP inhibitors. The rest? They’re left with chemotherapy that helps a little, but rarely enough.

Why Do Some Survive?
Every now and then, someone beats the odds. A 68-year-old woman in Manchester was diagnosed with stage IV pancreatic cancer in 2020. She had no surgery. She didn’t respond to first-line chemo. But she joined a trial for a combination of immunotherapy and a stroma-breaking drug. Two years later, her tumors were gone. No trace left.
She’s rare. But her case isn’t an anomaly-it’s a clue. Researchers are now studying her tumor’s genetic profile, her immune response, even her gut bacteria. They’re trying to figure out what made her different. Was it her diet? Her genes? The timing of treatment? No one knows yet. But her survival gives scientists something they’ve been starving for: a real-world example of what a cure might look like.
What Can You Do?
If you’re worried about pancreatic cancer, here’s what actually matters:
- Don’t smoke. Smoking doubles your risk.
- Maintain a healthy weight. Obesity raises your risk by 20%.
- Limit alcohol. Heavy drinking causes chronic pancreatitis, a known risk factor.
- Know your family history. If two or more close relatives had pancreatic cancer, talk to a genetic counselor.
- Don’t ignore unexplained weight loss, new-onset diabetes after 50, or persistent belly pain.
There’s no magic bullet. But catching it early-even if it’s rare-gives you the best shot.
Where Does Research Go From Here?
Scientists are now building national registries to track every case of pancreatic cancer in real time. They’re using AI to scan CT scans for early signs invisible to the human eye. Some labs are growing patient tumors in the lab to test dozens of drug combinations before giving them to the patient.
One UK-based project, the Pancreatic Cancer Research Fund’s Precision Medicine Initiative, is sequencing tumors from over 1,000 patients to find patterns. They’ve already identified three new subtypes that respond differently to treatment. That’s huge. It means the future won’t be one-size-fits-all chemo. It’ll be personalized, precise, and targeted.
It’s not going to happen overnight. But for the first time, researchers are seeing a path forward-not just more drugs, but smarter ones. And that’s the real breakthrough.
Is pancreatic cancer always fatal?
No, but it’s the most likely to be. About 12% of people live five years or more after diagnosis. That number rises to nearly 40% if the cancer is caught before it spreads beyond the pancreas. Early detection is rare, but when it happens, survival improves dramatically.
Can pancreatic cancer be cured with surgery?
Surgery is the only known path to a cure, but only 15% to 20% of patients are candidates. The tumor must be confined to the pancreas and not wrapped around major blood vessels. Even after successful surgery, most patients still need chemotherapy to kill any remaining cells. Recurrence is common.
Why doesn’t chemotherapy work well for pancreatic cancer?
The tumor is surrounded by a thick layer of scar tissue called stroma that blocks drugs from reaching cancer cells. The cancer also evolves quickly, developing resistance to treatments. Plus, many patients are too weak to tolerate full doses of chemo because the disease itself drains their energy and nutrition.
Are there any screening tests for pancreatic cancer?
No routine screening test exists for the general public. High-risk individuals-like those with inherited gene mutations or a strong family history-may get annual MRIs or endoscopic ultrasounds. But these are expensive, invasive, and not widely available.
What’s the difference between pancreatic cancer and pancreatitis?
Pancreatitis is inflammation of the pancreas, often caused by alcohol or gallstones. It’s painful but usually treatable. Pancreatic cancer is malignant growth of cells in the pancreas. While chronic pancreatitis increases cancer risk, most people with pancreatitis never develop cancer.
Can lifestyle changes reduce the risk of pancreatic cancer?
Yes. Quitting smoking cuts your risk by half. Maintaining a healthy weight, eating more vegetables and whole grains, and limiting red meat and processed foods can lower your risk by up to 25%. These changes won’t guarantee prevention, but they’re the best tools we have right now.
There’s no sugarcoating it: pancreatic cancer is the toughest cancer to cure. But science is learning. Every new discovery, every surviving patient, every gene mapped-these are pieces of a puzzle we’re finally starting to solve. The road ahead is long, but it’s no longer empty.