Pain Management Calculator for Open Heart Surgeries
Estimate Your Postoperative Pain Level
Estimated Pain Level
Your estimated pain level during recovery
Pain Management Summary
This tool estimates pain levels based on clinical studies. Actual pain may vary based on individual factors and specific surgical circumstances.
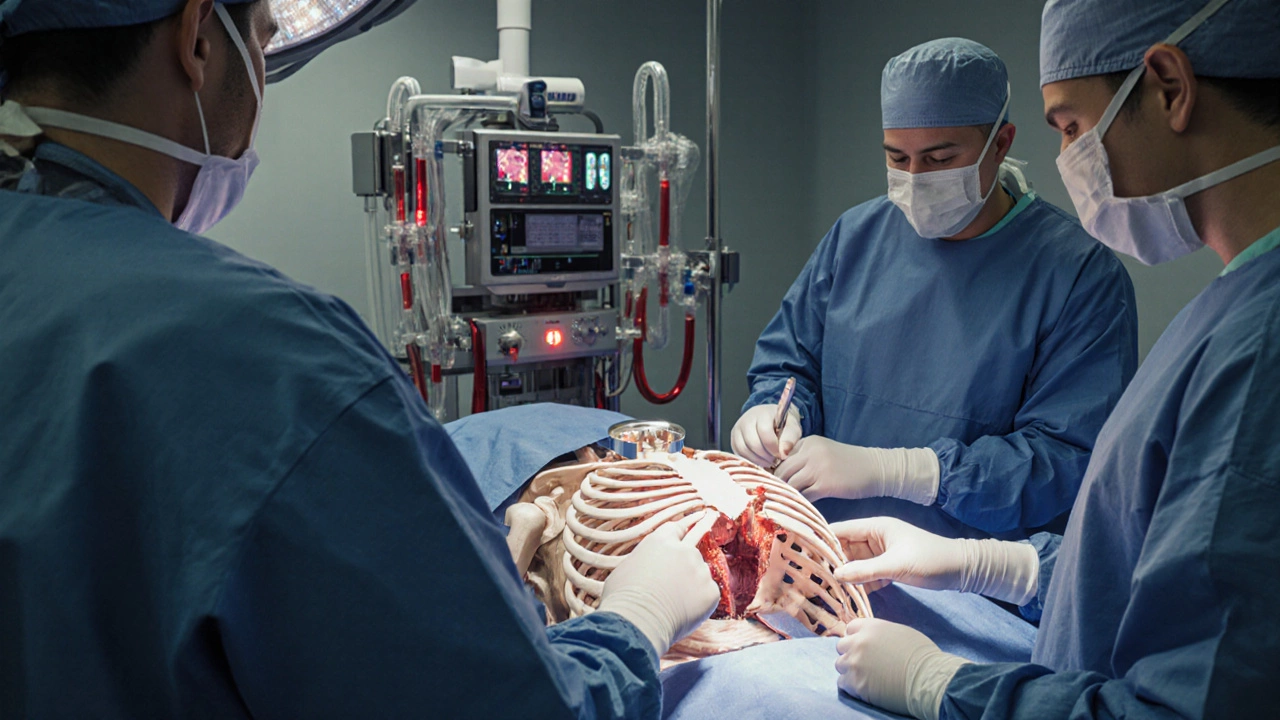
When doctors talk about the toughest operations, two procedures consistently top the list for raw, postoperative pain. Both involve opening the chest, stopping the heart, and working on the organ that never takes a break. The result? A recovery that feels like a marathon of soreness, fatigue, and emotional strain.
Why chest‑opening surgeries are so painful
To understand the intensity, you need to know what the body endures. A Open-heart surgery is a procedure that requires a full sternotomy (splitting the breastbone), placing the patient on cardiopulmonary bypass, and temporarily stopping the heart to access coronary arteries or valves. This means cutting through bone, pulling muscles, and interrupting blood flow for up to several hours.
When the bone is split, nerves in the periosteum (the layer covering bone) are exposed. Those nerves are extremely sensitive, and the inflammatory response that follows the incision can last weeks. Add to that the irritation from the heart‑lung machine, the need for multiple tubes in the chest, and the heavy use of analgesics, and you have a perfect storm of pain triggers.
The two surgeries that consistently rank as the most painful
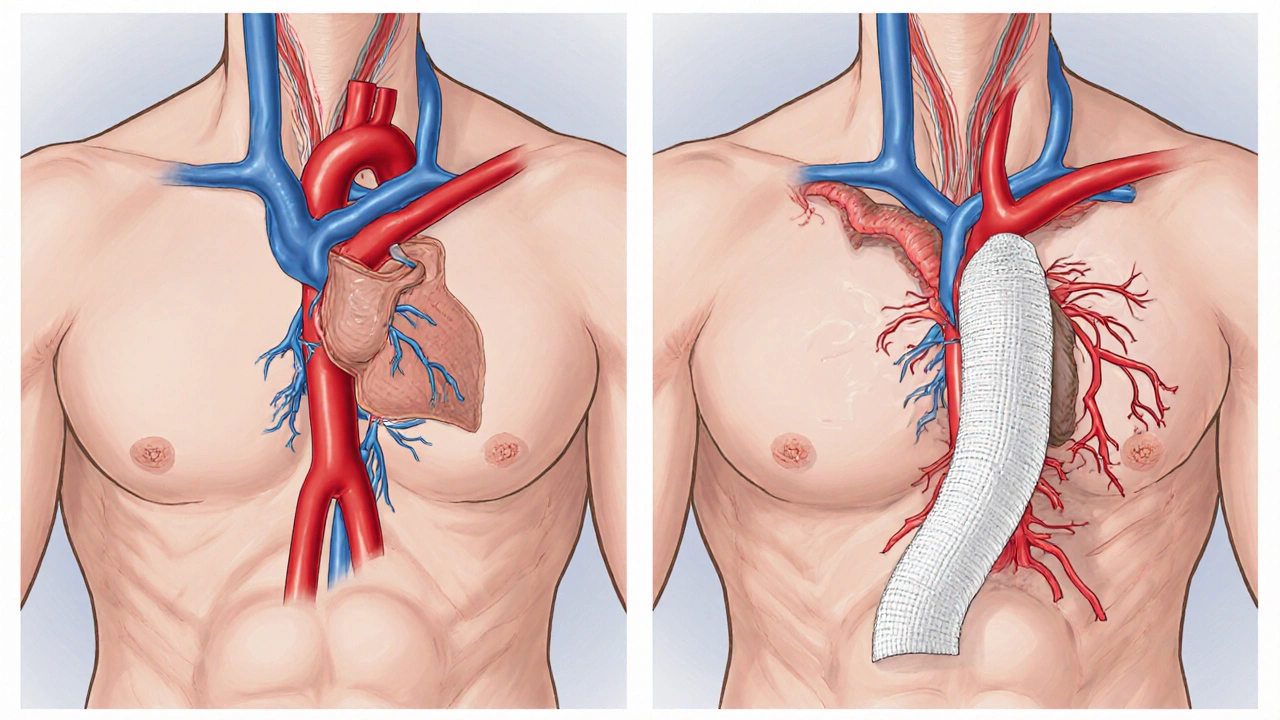
- Coronary Artery Bypass Grafting (CABG) - a classic open‑heart operation where surgeons harvest vessels from the leg or chest and graft them onto blocked coronary arteries.
- Open Thoracic Aortic Aneurysm Repair - a major operation that replaces a weakened section of the aorta with a synthetic graft, also requiring a full sternotomy and often deep hypothermic circulatory arrest.
Both procedures share the same painful elements-sternotomy, cardiopulmonary bypass, and a lengthy ICU stay-yet each has its own nuances that affect the pain profile.
Coronary Artery Bypass Grafting (CABG)
In a CABG, the surgeon creates a new route for blood to flow around narrowed coronary arteries. The most common graft source is the internal mammary artery, but the leg’s saphenous vein is also used.
- Surgical incision: A vertical split down the breastbone (sternotomy) about 12cm long.
- Typical operative time: 3-5hours, plus time on the heart‑lung machine.
- Hospital stay: 5-7days in the ICU and regular ward before discharge.
Patients often report a sharp, burning sensation around the sternum that peaks between days2‑4. A study from the Journal of Cardiac Surgery (2023) found that 68% of CABG patients rated their pain as >7 on a 10‑point visual analogue scale (VAS) during the first 48hours.
Why is the pain that high? The sternotomy cuts through both the cortical bone and the periosteum, which is densely innervated. The heart‑lung machine also triggers a systemic inflammatory response, worsening muscle soreness.
Open Thoracic Aortic Aneurysm Repair
When a section of the aorta swells beyond safe limits, surgeons replace it with a synthetic graft. The operation is technically demanding because the aorta sits deep behind the heart and lungs.
- Surgical incision: Same full sternotomy, but the opening is often extended laterally to improve access.
- Operative time: 5-8hours, sometimes longer if hypothermic circulatory arrest is needed.
- Hospital stay: 7-10days, with a longer ICU period due to the complexity of the repair.
Patients describe the pain as a “deep ache” that radiates from the chest to the upper back. The same 2023 cardiac journal reported an average VAS score of 8.2 for the first 72hours, slightly higher than CABG because of the longer operation and the need for more extensive tissue retraction.
Another factor is the “reperfusion injury” that occurs when blood flow is restored to the aorta. This can cause additional inflammation and muscle spasm, adding to the pain burden.
How pain is measured and why it matters
Clinicians use the Visual Analogue Scale (VAS) and the Numeric Rating Scale (NRS) to quantify pain. Both ask patients to rate their discomfort on a 0-10 scale, where 0 is no pain and 10 is the worst imaginable.
Accurate pain measurement is crucial because undertreated pain can lead to chronic post‑sternotomy pain syndrome (PSPS). PSPS affects up to 25% of patients one year after surgery and manifests as persistent aching, numbness, or hypersensitivity at the scar site.
To prevent PSPS, hospitals now adopt multimodal analgesia-using several drugs and techniques together to hit different pain pathways.
Multimodal pain‑management strategies
Here’s what most cardiac centers do to tame the sting of a sternotomy:
- Epidural or paravertebral block: An anesthetic is placed near the spinal nerves before the incision. Studies show a 30% reduction in opioid consumption.
- Intravenous acetaminophen: Helps lower the VAS by 1‑2 points without affecting blood clotting.
- Non‑steroidal anti‑inflammatory drugs (NSAIDs): Use is limited because they can interfere with platelet function, but low‑dose ibuprofen is often safe after the first 24hours.
- Opioid‑sparing protocols: Short‑acting opioids like sufentanil are given via patient‑controlled analgesia (PCA) for breakthrough pain.
- Local anesthetic infiltration: Surgeons spray ropivacaine directly onto the sternum before closing, extending analgesia for up to 12hours.
Physical therapy starts on day1 to promote deep breathing and prevent lung complications, but gentle movement also helps keep the chest wall from stiffening, which can worsen pain.
Recovery timeline: what to expect after each surgery
| Aspect | Coronary Artery Bypass Grafting (CABG) | Open Thoracic Aortic Aneurysm Repair |
|---|---|---|
| Average operative time | 3-5hours | 5-8hours |
| ICU stay | 1-2days | 2-4days |
| Hospital discharge | 5-7days | 7-10days |
| Peak VAS pain score (first 72h) | 7.2±1.1 | 8.2±1.3 |
| Typical analgesic regimen | Epidural + IV acetaminophen + PCA opioids | Epidural + higher‑dose opioids + local ropivacaine |
| Incidence of chronic PSPS (12months) | 22% | 28% |
Both surgeries demand patience. Most patients can return to light daily activities after 6-8weeks, but full‑strength exercise often takes 3-4months. The key is adhering to the cardiac rehab program and keeping pain under control; lingering soreness can discourage patients from staying active.

Real‑world patient stories that illustrate the pain
John, 58, a former smoker, had a triple‑vessel CABG. “The first night felt like someone was hammering my chest,” he recalls. “By day3 the pain was still a 7, and the opioids made me feel foggy. The epidural saved me; after it was removed, I could finally breathe without wincing.”
Maria, 62, underwent open aortic repair for a 6cm aneurysm. “I expected a lot of pain, but the back‑radiating ache was brutal. I was on a PCA pump for a week, and the physiotherapist’s gentle breathing exercises were the only thing that kept my lungs clear.”
These anecdotes echo the clinical data: aggressive, multimodal pain control is not a luxury-it’s a necessity for a smoother recovery.
Key takeaways
- The two surgeries that consistently rank as the most painful are coronary artery bypass grafting and open thoracic aortic aneurysm repair.
- Both involve a sternotomy, cardiopulmonary bypass, and a high inflammatory response, which together drive VAS scores above 7.
- Multimodal analgesia-epidural blocks, IV acetaminophen, limited NSAIDs, and careful opioid use-cuts pain scores by about a third.
- Recovery is a marathon, not a sprint; expect 6‑8weeks for light activity and up to 4months for full exercise capacity.
- Untreated pain can lead to chronic post‑sternotomy pain syndrome, underscoring the need for proactive pain management.
Frequently Asked Questions
What makes a sternotomy so painful?
Cutting through the breastbone damages the periosteum, which is densely packed with pain fibers. The bone also heals slowly, and the inflammatory response from the heart‑lung machine adds muscle soreness.
Can I avoid opioids after these surgeries?
Many centers use opioid‑sparing protocols that combine epidurals, acetaminophen, and local anesthetic infiltration. While some short‑acting opioids are still used for breakthrough pain, the overall dose can be reduced by 30‑50%.
How long does the risk of chronic post‑sternotomy pain last?
If pain isn’t well‑controlled in the first 3months, the likelihood of chronic symptoms rises. Up to 25% of patients still report noticeable chest discomfort a year after surgery.
Is an endovascular (stent‑graft) approach less painful than open aortic repair?
Yes. Endovascular repair avoids a sternotomy and usually requires a smaller incision, resulting in lower VAS scores (average 4‑5) and a shorter hospital stay.
When can I return to normal exercise after CABG?
Light activities are safe after 6weeks, but most cardiologists advise a supervised cardiac rehab program for at least 12weeks before resuming high‑intensity workouts.
Understanding which surgeries cause the most pain-and why-helps patients prepare mentally, set realistic expectations, and work with their care team to choose the right pain‑control plan. Armed with that knowledge, the journey from the operating table to a full, active life becomes far less intimidating.