IVF Timing Calculator
IVF Timing Calculator
Calculate your personalized waiting period before starting IVF after childbirth based on delivery type, breastfeeding status, age, and other factors.
Recommended Waiting Period
Key Considerations:
- Uterine healing needs time, especially after C-sections
- Hormonal balance takes time to stabilize
- Age may shorten recommended waiting period
- Previous IVF cycles may require extra recovery time
Important Note: This calculator provides general guidelines. Always consult with your fertility specialist for personalized medical advice.
When couples wonder IVF (In Vitro Fertilization) is a lab‑based assisted reproductive technology that combines eggs and sperm outside the body to create embryos, timing after a recent birth can feel confusing. The good news? Most specialists agree there’s a safe window, but the exact number of weeks depends on a handful of personal factors.
Quick Takeaways
- Medical bodies usually recommend waiting at least 3 months after a vaginal birth and 6 months after a Caesarean before starting IVF.
- Breastfeeding, hormone levels, and uterine healing are the biggest variables.
- Age, previous IVF cycles, and underlying health conditions can push the waiting period to 12 months or more.
- Pre‑IVF testing (ultrasound, hormone panel, sperm analysis) should be done well before the first medication cycle.
- Emotional readiness matters - give yourself and your partner space to adjust to life with a new baby.
Understanding the Post‑partum Body
The postpartum period refers to the weeks and months after childbirth when the mother’s body returns to its pre‑pregnancy state. During this time the uterus, which stretched to accommodate a growing baby, shrinks back to roughly the size of a fist. Hormonal fluctuations are massive: levels of estrogen a primary female sex hormone that regulates the menstrual cycle and progesterone supports pregnancy and prepares the uterine lining for implantation dip sharply, while prolactin a hormone that promotes milk production and suppresses ovulation spikes if you’re nursing. These swings affect both fertility and how your body reacts to IVF drugs.
What the Guidelines Say
Two major authorities give clear, evidence‑based advice:
- American Society for Reproductive Medicine (ASRM) the leading US professional organization for infertility specialists suggests a minimum of 3 months after a vaginal delivery and 6 months after a Caesarean before initiating ovarian stimulation.
- The UK’s NICE National Institute for Health and Care Excellence, which issues clinical guidelines for the NHS recommends a similar 3‑month buffer, but adds that women who are still breastfeeding may need a longer pause to avoid medication‑related milk suppression.
These timelines aren’t arbitrary; they protect the uterus from premature stress, give hormone levels a chance to stabilize, and let the doctor assess any lingering complications.
Factors That Can Shorten or Lengthen the Waiting Period
Even with clear baseline numbers, real‑life decisions hinge on several personal variables:
- Age - Women over 35 see a faster decline in ovarian reserve the quantity and quality of a woman’s remaining eggs. If time is of the essence, some clinics may start treatment after a 2‑month wait, provided the uterus looks healthy.
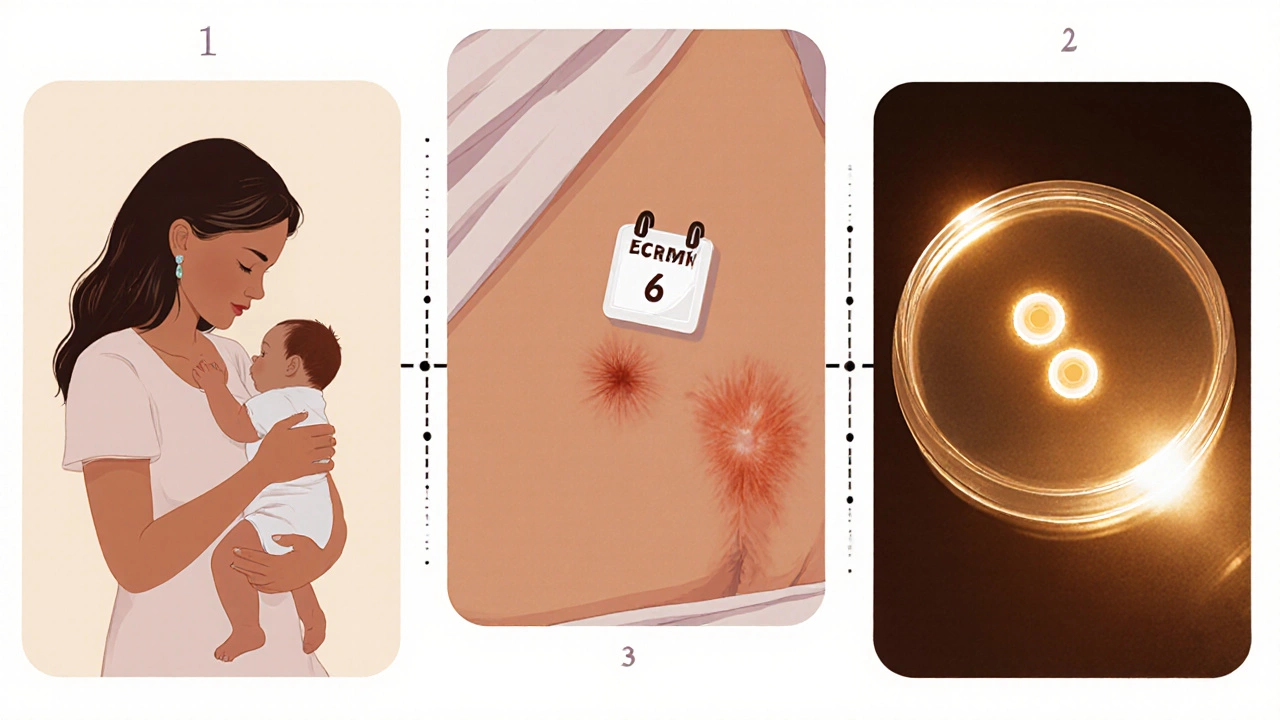
- Delivery type - A Caesarean section involves a surgical scar on the uterus. Healing can take up to 6 months, so most doctors advise the longer interval.
- Breastfeeding - While nursing offers many health benefits, high prolactin can suppress ovulation and interfere with the ovarian‑stimulation drugs used in IVF. Some women choose to wean before starting.
- Previous IVF attempts - If you’ve already gone through a cycle that failed, a short “break” can give your body a chance to recover from aggressive hormone doses.
- Overall health - Conditions like thyroid disorders, uncontrolled diabetes, or severe anemia need treatment first. They can push the start date back by weeks or months.
Typical Recommended Intervals - A Quick Comparison
| Scenario | Minimum Wait | Reasoning |
|---|---|---|
| Vaginal delivery, not breastfeeding | 3 months | Uterine contraction complete, hormones stabilizing |
| Vaginal delivery, exclusive breastfeeding | 4-6 months | High prolactin levels may inhibit ovarian response |
| Caesarean section, any feeding mode | 6 months | Surgical scar needs full healing before stimulation drugs |
| Maternal age > 35 or low ovarian reserve | 2-3 months (if uterus healthy) | Time‑sensitivity outweighs longer healing concerns |
| Previous IVF cycle within 6 months | 3 months | Allow body to recover from high‑dose hormones |
Preparing for IVF After a Baby
Once you’ve settled on a timeline, the next step is preparation. Most clinics ask for these baseline tests:
- Transvaginal ultrasound - Checks the thickness of the uterine lining the inner tissue of the uterus where an embryo would implant and counts antral follicles to gauge ovarian reserve.
- Hormone panel - Measurements of FSH Follicle‑stimulating hormone, a key indicator of egg quality, AMH Anti‑Müllerian hormone, another marker of egg supply, and thyroid‑stimulating hormone (TSH).
- Semen analysis - Partner’s sperm count, motility, and morphology must be within acceptable ranges; otherwise, you might need ICSI (intracytoplasmic sperm injection).
- General health screen - Blood pressure, BMI, and any chronic disease status are reviewed to ensure safe medication dosing.
While you’re waiting, focus on a balanced diet rich in folate, iron, and omega‑3 fatty acids, stay active with low‑impact exercises, and aim for 7-8 hours of sleep each night. These steps improve both your own recovery and the environment your future embryo will grow in.
Risks of Starting Too Early
Jumping into a stimulation cycle before the body’s ready can lead to several issues:
- Uterine scar dehiscence - Rare but serious, especially after a C‑section. The uterus may thin out, raising the risk of miscarriage or ectopic implantation.
- Ovarian hyper‑response - Hormone levels are already shifting; adding aggressive medication can cause swelling, pain, and in extreme cases, ovarian‑torsion.
- Emotional burnout - Juggling newborn care, possible breastfeeding, and a demanding IVF schedule can sap mental stamina, lowering overall success rates.
That’s why your fertility specialist will often run a quick ultrasound before the first medication dose, just to confirm the uterus looks healthy.
Real‑World Stories
Case A: Maya, 32, delivered a healthy baby via vaginal birth. She stopped breastfeeding at 4 months, waited 3 months, and started a standard IVF cycle. Her uterus measured 9 mm thickness, and she achieved a fresh embryo transfer that resulted in a twin pregnancy.
Case B: Liam and Priya, 38 and 36, had a Caesarean delivery. Priya continued to breastfeed and wanted to try IVF quickly because of age concerns. After consulting with a specialist, they waited 6 months, weaned the baby, and opted for a mild‑dose IVF protocol. The cycle produced two top‑quality embryos, and one implanted successfully.
Both stories highlight the importance of customizing the waiting period to your health, delivery type, and personal goals.
Bottom Line - When Can You Start?
There’s no one‑size‑fits‑all answer, but most experts converge on these practical rules:
- If you had a vaginal birth and are not breastfeeding, 3 months is usually safe.
- If you’re still nursing, aim for at least 4-6 months to let prolactin settle.
- After a Caesarean section, give the scar 6 months to fully heal.
- Women over 35 or those with low ovarian reserve may need a shorter wait, provided the uterus is cleared for stimulation.
- Always get a baseline ultrasound and hormone panel before the first drug dose; the results will confirm whether you’re truly ready.
Talk to a qualified fertility doctor a specialist who evaluates reproductive health and designs IVF treatment plans to tailor the timeline to your specific situation. Remember, the best IVF outcome is a mix of timing, health, and emotional readiness.
Can I start IVF while still breastfeeding?
Many clinics advise waiting until prolactin levels drop, usually around 4-6 months postpartum. Some women do start earlier with a mild‑dose protocol, but they risk lower ovarian response and may need to pause breastfeeding temporarily.
What if I had a C‑section?
A Caesarean creates a uterine scar that typically needs 6 months to heal fully. Starting IVF earlier can increase the chance of scar dehiscence and implantation problems, so most specialists recommend waiting the full six months.
Does maternal age change the waiting time?
Yes. Women over 35 often have a faster decline in ovarian reserve. If the uterus is healthy, doctors may allow a shorter 2‑month wait to avoid losing precious time.
What tests should I do before the first IVF cycle?
A transvaginal ultrasound, hormone panel (FSH, AMH, TSH), semen analysis for the partner, and a general health check (BP, BMI, chronic conditions) are standard. These results guide the medication dosage and timing.
Is it safe to combine IVF with a newborn at home?
It’s possible, but support is crucial. IVF medications can cause fatigue, mood swings, and occasional abdominal discomfort. Having a partner, family member, or doula to help with the baby can make the process smoother.