Diabetes Medication Decision Guide
Personalized Recommendation Tool
Answer these questions to find the best metformin alternative for your situation.
What is your eGFR (ml/min/1.73m²)?
Do you have established cardiovascular disease or heart failure?
What is your primary goal?
Do you prefer oral medications over injections?
Quick Takeaways
- Metformin works well for many, but there are several drug classes that can be a better fit depending on weight, heart health, or kidney function.
- SGLT2 inhibitors and GLP‑1 receptor agonists lead the pack for cardiovascular protection.
- Consider side‑effect profiles, cost, and how the medication matches your lifestyle.
- Always discuss any switch with your healthcare provider.
When you hear “metformin,” you probably think of the first‑line pill for type2 diabetes. It’s cheap, well‑studied, and helps control blood sugar without causing hypoglycemia. But metformin isn’t a one‑size‑fits‑all solution. Some people can’t tolerate its gastrointestinal side effects, others have kidney issues that limit its use, and a growing number of patients need a medication that also protects their heart or helps them lose weight. That’s where metformin alternatives come into play.
Understanding Metformin’s Role
Metformin is a biguanide oral medication that lowers blood glucose by reducing hepatic glucose production and improving insulin sensitivity. It’s recommended by most guidelines as the first drug after lifestyle changes. Typical doses range from 500mg to 2,000mg per day, taken with meals to reduce nausea.
While metformin shines in many areas-low cost, modest weight loss, and a solid safety record-not everyone can stay on it. Common reasons to look for a different drug include:
- Persistent stomach upset or diarrhea despite dose adjustments.
- Renal impairment (eGFR below 45ml/min/1.73m²) that makes metformin unsafe.
- Need for additional cardiovascular risk reduction beyond glucose control.
- Desire for more pronounced weight loss.
When Metformin May Not Be Ideal
If you fall into any of the categories above, your doctor will likely explore other drug classes. The modern diabetes pharmacopeia offers at least six major alternatives, each with its own mechanism and side‑effect profile.

Main Classes of Alternatives
Below are the big players you’ll hear about during a clinic visit.
SGLT2 inhibitors are a class that block sodium‑glucose co‑transporters in the kidney, causing excess glucose to be expelled in the urine. Examples include empagliflozin, canagliflozin, and dapagliflozin.
GLP‑1 receptor agonists mimic the incretin hormone glucagon‑like peptide‑1, enhancing insulin secretion, slowing gastric emptying, and promoting satiety. Popular agents are liraglutide, semaglutide, and dulaglutide.
DPP‑4 inhibitors work by preventing the breakdown of endogenous GLP‑1, thereby modestly boosting insulin release. Sitagliptin and saxagliptin are common choices.
Other options include thiazolidinediones (e.g., pioglitazone), sulfonylureas (e.g., glipizide), and injectable insulin for people who need more aggressive control.
Detailed Comparison Table
| Drug class | Example(s) | Primary mechanism | Weight impact | Cardiovascular benefit | Typical side effects |
|---|---|---|---|---|---|
| SGLT2 inhibitors | Empagliflozin, Canagliflozin | Blocks kidney glucose reabsorption | Modest loss (1‑3kg) | Reduced CV death & HF hospitalization | UTI, genital infections, dehydration |
| GLP‑1 receptor agonists | Liraglutide, Semaglutide | Enhances insulin, slows gastric emptying | Significant loss (3‑6kg) | Lowered MACE risk, stroke reduction | Nausea, vomiting, pancreatitis (rare) |
| DPP‑4 inhibitors | Sitagliptin, Saxagliptin | Prevents GLP‑1 breakdown | Neutral | Neutral | Headache, nasopharyngitis |
| Thiazolidinediones | Pioglitazone | Improves peripheral insulin sensitivity | Weight gain (2‑3kg) | Possible CV benefit in some trials | Edema, heart‑failure risk, bone loss |
| Sulfonylureas | Glipizide, Glyburide | Stimulates pancreatic insulin release | Neutral or slight gain | Neutral | Hypoglycemia, weight gain |
| Basal insulin | Insulin glargine, Detemir | Provides steady exogenous insulin | Neutral or slight gain | Neutral | Hypoglycemia, weight gain |
How to Choose the Right Alternative
Picking a drug isn’t just about the table. Think about these practical factors:
- Kidney function. SGLT2 inhibitors need eGFR≥45ml/min for full benefit; below that, dose may be reduced or the drug avoided.
- Cardiovascular profile. If you have heart failure or established ASCVD, an SGLT2 inhibitor or GLP‑1 agonist is usually preferred.
- Weight goals. GLP‑1 agonists are the only class that consistently produces meaningful weight loss.
- Cost and insurance coverage. Metformin is cheap; many newer agents are pricier, though some generic SGLT2 inhibitors have entered the market in 2024.
- Administration route. Oral options (SGLT2, DPP‑4, thiazolidinediones) are easier for those averse to daily injections, but weekly GLP‑1 pens may improve adherence for busy patients.
- Side‑effect tolerance. If you’ve struggled with GI upset on metformin, you might welcome the lower GI burden of an SGLT2 inhibitor, but be prepared for potential genital infections.
A simple decision tree can help:
- Do you have heart failure or ASCVD? → Consider SGLT2 inhibitor first.
- Is weight loss a priority? → GLP‑1 receptor agonist is the top choice.
- Is your eGFR below 45? → Avoid SGLT2 inhibitors; look at DPP‑4 inhibitors or low‑dose insulin.
- Do you prefer an oral tablet? → SGLT2, DPP‑4, thiazolidinediones, or sulfonylureas.
Lifestyle Factors & Medication Synergy
No drug works in isolation. Pairing the right medication with diet, exercise, and sleep improves outcomes dramatically. For example, combining a GLP‑1 agonist with a low‑carb diet can amplify weight loss, while an SGLT2 inhibitor paired with moderate aerobic activity boosts cardiovascular fitness.
Monitoring is key. Keep a log of fasting glucose, post‑meal spikes, and any side effects. Modern apps can send data directly to your clinic, allowing quick dose tweaks.
When to Talk to Your Doctor
You should schedule a review if you notice any of the following:
- Persistent nausea, vomiting, or diarrhea that interferes with daily life.
- Signs of urinary or genital infection - redness, itching, foul odor.
- Unexplained swelling in the legs or shortness of breath (possible heart‑failure signal).
- Blood sugar consistently above target despite medication adherence.
- Changes in kidney function tests.
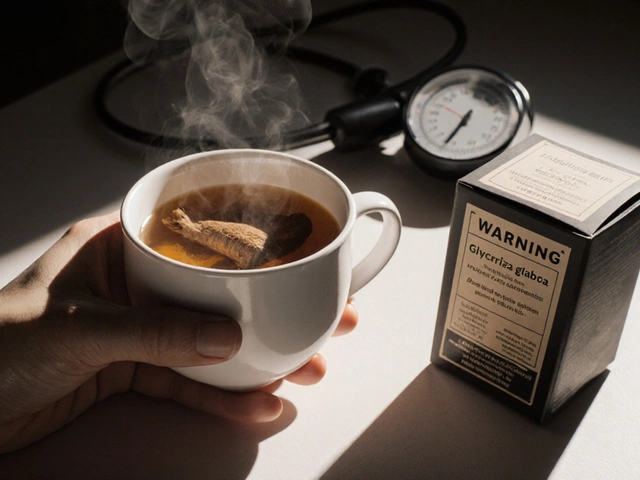
Bring recent lab results, a list of current meds (including over‑the‑counter supplements), and any lifestyle changes you’ve made. This information helps the clinician tailor a regimen that fits your unique picture.
Frequently Asked Questions
Can I take an SGLT2 inhibitor while on metformin?
Yes. Many guidelines recommend adding an SGLT2 inhibitor to metformin for extra heart protection and glucose lowering. Your doctor will check kidney function first.
Do GLP‑1 agonists cause low blood sugar?
Rarely. Since they work only when glucose is high, they have a low risk of hypoglycemia unless combined with insulin or a sulfonylurea.
What if I have a low eGFR?
When eGFR falls below 45ml/min, SGLT2 inhibitors lose effectiveness and may be unsafe. DPP‑4 inhibitors or a low‑dose insulin regimen become safer alternatives.
Are there generic versions of these newer drugs?
As of 2024, generic empagliflozin and dapagliflozin are available in many markets, reducing cost substantially. Generic GLP‑1 agents are still pending regulatory approval.
How quickly can I expect weight loss with a GLP‑1 agonist?
Patients often lose 3‑5kg in the first three months, with continued loss up to 10kg over a year if diet and activity are supportive.