Knee Replacement Readiness Calculator
How much is your knee limiting your life?
Answer these 7 questions based on your experience. Your score will show if it's time to see a specialist.
Most people don’t wake up one day and decide they need a knee replacement. It creeps up. First, it’s just stiffness after sitting too long. Then, it’s pain climbing stairs. Soon, walking to the mailbox feels like a marathon. You start avoiding things you used to love-gardening, playing with grandkids, even Sunday walks. But when is it knee replacement time? Not too early. Not too late. Just right.
It’s Not Just About Pain
Pain is the loudest signal, but it’s not the only one. Some people have severe X-rays and feel fine. Others have mild arthritis and can’t stand up without gritting their teeth. What matters more is how much your knee is stealing your life.
Think about your daily routine. Can you get out of bed without holding onto something? Can you stand in the kitchen to make tea without needing a chair? If you’re using a cane just to walk to the bathroom, or if you’ve stopped going to the gym because your knee gives out halfway through, those aren’t just inconveniences. They’re red flags.
A study from the University of Oxford followed 1,200 people with osteoarthritis over five years. Those who waited until their pain was constant-day and night, even at rest-had worse outcomes after surgery. Why? Because their muscles had weakened, their gait had changed, and their bodies had adapted to moving wrong. Surgery works best when you’re still strong enough to bounce back.
When Movement Starts to Fail
Your knee isn’t just a hinge. It’s part of a system. When it breaks down, everything else compensates. You lean to one side. You shorten your stride. You start limping. That’s not just discomfort. That’s body damage waiting to happen.
If you’ve noticed your knee locking up-suddenly stuck, like it’s jammed-you’re likely dealing with a torn meniscus or loose cartilage. If it pops or grinds loudly when you stand, that’s bone-on-bone. If you can’t fully straighten your leg or bend it past 90 degrees, your joint is losing function. These aren’t normal signs of aging. They’re signs your knee is failing.
One patient I saw last year, a 68-year-old retired teacher, stopped teaching yoga because she couldn’t get up from the floor. She didn’t complain about pain much, but she cried when she said, “I can’t hug my grandchildren like I used to.” That’s the moment you need to listen to-not just your knee, but your life.
Medications and Injections Aren’t Fixing It
Anti-inflammatories, knee braces, physical therapy, cortisone shots-these all help. For a while. But if you’re going through a new round of injections every three months just to get through the week, you’re managing, not healing.
There’s a limit to how many steroid injections your joint can take. Most doctors won’t give more than three or four a year. If you’ve hit that limit and still can’t walk without pain, the cartilage is likely gone. No amount of gel or pill will grow it back.
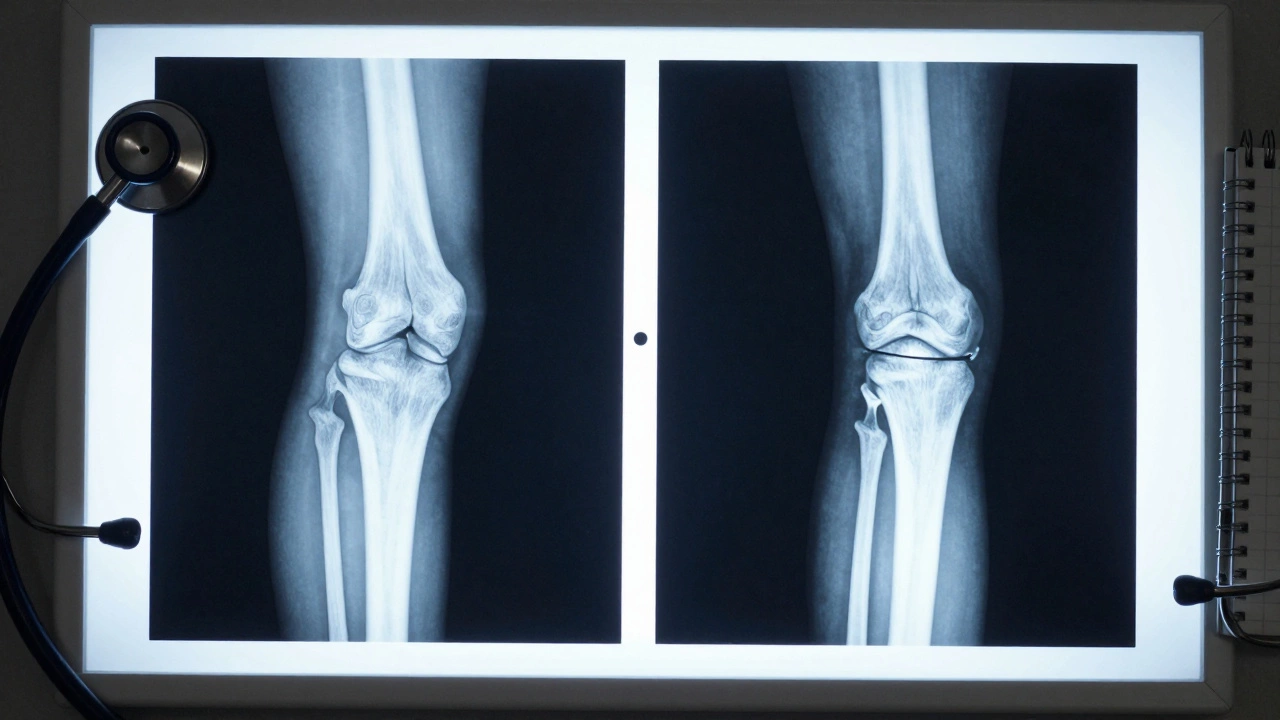
Viscosupplementation (hyaluronic acid shots) works for some, especially in early stages. But if your X-ray shows the space between your bones is nearly gone-less than 2 millimeters-you’re past the point where injections help. That’s not a guess. That’s measurable on an MRI or weight-bearing X-ray.

The Night Pain Test
Here’s a simple rule many orthopedic surgeons use: if your knee wakes you up at night, it’s time to talk about surgery.
Pain that only happens when you’re active? That’s manageable. Pain that keeps you up at 3 a.m.? That means inflammation is constant. Your body isn’t getting a break. Your nervous system is stuck in overdrive. That’s a sign your joint is in chronic failure mode.
One woman I met in London, a 72-year-old former nurse, said she started sleeping in a recliner because lying flat made her knee throb. She’d been told to “wait until it’s unbearable.” But unbearable wasn’t the goal. The goal was to get her back to her garden, her book club, her morning coffee on the porch. She had surgery. Six weeks later, she was planting tulips again.
What Happens If You Wait Too Long?
Waiting doesn’t make your knee better. It just makes recovery harder.
When you avoid movement because of pain, your thigh muscles shrink. The quadriceps can lose up to 40% of their strength in six months. That means your new knee won’t have the support it needs. Rehab becomes longer. Progress slower. Risk of complications higher.
Also, your other joints suffer. Your hip, your ankle, your lower back-they all start to take extra strain. One study found that people who delayed knee replacement by more than two years after symptoms became severe had a 30% higher chance of needing hip or spine treatment within five years.
And then there’s the mental toll. Chronic pain changes your brain. It lowers your tolerance for stress, makes you more anxious, and can even lead to depression. Surgery isn’t just about fixing a joint. It’s about reclaiming your peace of mind.
When It’s Not Time Yet
Not everyone with knee pain needs surgery. Some people have mild to moderate arthritis and still live full lives. If you can walk a mile, climb stairs without stopping, sleep through the night, and manage pain with occasional ibuprofen or a heat pack-you’re not ready.
Try this: commit to three months of physical therapy, weight management (even 5% loss helps), and low-impact exercise like swimming or cycling. If your pain doesn’t improve, or if your mobility gets worse, then it’s time to revisit surgery.
Some people think they need a knee replacement because they have “bone-on-bone” on an X-ray. But X-rays don’t show pain. They show structure. Two people can have the same X-ray and feel completely different. That’s why your symptoms matter more than the scan.
What to Expect After Surgery
Modern knee replacements last 20 to 25 years for most people. Recovery isn’t easy, but it’s predictable. Most people walk with a cane in two weeks. By six weeks, they’re driving. By three months, they’re back to walking, gardening, even light hiking.
Success isn’t about running marathons. It’s about putting on your own shoes. Getting into the car without help. Standing at the sink without holding on. Those are the wins that matter.
There’s no magic age. I’ve seen 50-year-olds with severe arthritis from sports injuries and 80-year-olds with barely any pain. It’s not about how old you are. It’s about how much your knee is holding you back.
Next Steps: What to Do Now
- Track your pain for two weeks. Use a simple scale: 1 (barely there) to 10 (unbearable). Note when it happens and what makes it better or worse.
- Try a 30-minute walk every day. If you can’t do it without pain that lasts more than two hours, that’s a sign.
- See an orthopedic specialist. Bring your X-rays and a list of what you can’t do anymore.
- Ask about the Kellgren-Lawrence scale. It’s the standard way doctors grade arthritis severity. Grade 3 or 4? That’s advanced.
- Don’t wait for the pain to be “bad enough.” Wait until your life is no longer working the way you want it to.
Your knee doesn’t need to be destroyed before you fix it. It just needs to be stopping you from living.
Is knee replacement only for older people?
No. While most patients are over 60, younger people with severe arthritis from injury, genetics, or autoimmune conditions also benefit. The key factor isn’t age-it’s function. If your knee is limiting your daily life, surgery can help regardless of how old you are.
Can I avoid surgery with physical therapy?
Yes, for many. Physical therapy can strengthen muscles around the knee, reduce pain, and improve mobility-especially in early to moderate arthritis. But if your cartilage is worn down to bone, therapy can’t rebuild it. It can only manage the symptoms. If therapy hasn’t helped after 3-6 months, surgery is likely the next step.
How long does recovery take after knee replacement?
Most people walk without a cane in 2-4 weeks. Driving returns around 4-6 weeks. Full recovery, including muscle strength and range of motion, takes 3-6 months. Many patients say they feel like themselves again by the three-month mark. Staying active during rehab is the biggest factor in how fast you heal.
Are there alternatives to full knee replacement?
Yes. Partial knee replacement works if only one side of the knee is damaged. Osteotomy, which realigns the leg to take pressure off the bad part, is an option for younger, active patients. But these are not for everyone. They require specific conditions and aren’t as long-lasting as a full replacement. Your surgeon can tell you which fits your case.
Will I ever be able to walk normally again?
Most people do. The goal isn’t to run a marathon-it’s to walk without pain, climb stairs, stand up from a chair, and get into the car without help. Studies show over 90% of patients report major improvements in mobility and quality of life after surgery. You won’t feel like you did at 25, but you’ll feel like yourself again.
What happens if I never get surgery?
Your knee will keep getting worse. Pain will increase. Mobility will decrease. You’ll lose muscle strength. You may start relying on walking aids. Your other joints-hips, back, ankles-will compensate and could develop problems too. Your quality of life will decline, and your risk of falls and injuries goes up. Surgery isn’t the only option, but delaying it often makes things harder.
Final Thought: It’s About Your Life, Not Just Your Knee
You don’t need to suffer in silence. You don’t need to wait until you’re in agony. You just need to ask yourself: Is my knee still letting me live the way I want to? If the answer is no, then it’s not too soon. It’s just in time.





