No one wants to hear the word 'incurable' when talking about cancer, but it's the honest reality for some types. This doesn't mean there’s zero hope, but it does mean doctors can’t promise to wipe out the cancer for good. People commonly ask which cancers fall into this category and what that means for treatment and everyday life.
Take pancreatic cancer, for example. Around 80% of patients only find out when it’s already spread, making surgery impossible. Or glioblastoma, a brain cancer so sneaky it keeps coming back even after aggressive treatment. These aren’t just rare exceptions. Several cancers—like some kinds of lung cancer or metastatic prostate cancer—tend to come back or stop responding to treatment at some point.
Learning about which cancers have no cure isn’t about losing hope. It’s about arming yourself with real info. It helps you ask the right questions, weigh your options, and maybe even find a kind of peace in the middle of chaos. Want to get a handle on what 'no cure' really means, what doctors actually can do, and how people keep fighting? Stick around—we’ll walk through it together.
- Why Some Cancers Have No Cure
- Uncurable Cancers—A Closer Look
- Modern Treatments: What’s Possible, What’s Not
- Living with an Incurable Diagnosis
- Breakthroughs and Hope on the Horizon
- Tips for Patients and Families
Why Some Cancers Have No Cure
It probably sounds unfair, but not every cancer can be fully wiped out by today’s treatment. There’s no big mystery behind it—just a bunch of frustrating realities. The main problem boils down to how sneaky and stubborn some cancers are. They spread fast, they dodge treatments, and sometimes, by the time you even spot them, they’ve already set up shop in more than one part of the body. When doctors call a cancer "incurable," they basically mean treatments can shrink it or slow it down, but they can’t promise it’ll ever be truly gone for good.
With uncurable cancer, there are a few big reasons why a cure just isn’t on the table right now:
- Late diagnosis: Some cancers, like pancreatic or ovarian, show up without obvious symptoms until they’re already advanced and have spread.
- Location: Tumors in hard-to-reach spots (think brain or spinal cord) can hide from surgery or radiation.
- Mutation tricks: Certain cancers evolve quickly, dodging the drugs thrown at them. For example, lung cancer cells can change, making them resistant to treatment.
- Spread: Metastatic cancer (when it’s traveled beyond its starting point) is much harder to get under control.
Check this out: according to the American Cancer Society, about 60% of all terminal cancer diagnoses are discovered after they've already spread beyond the original site. That’s a huge reason why so many cases don’t have a cure.
"Despite new therapies, some cancers are still considered incurable due to late diagnosis and rapid spread. Managing symptoms and quality of life becomes the main focus." — Dr. Rebecca Siegel, American Cancer Society
So, this doesn’t mean people just sit back and accept it. Treatments are still worth it—they can add time, shrink tumors, and help folks feel better. It’s just that right now, for certain cancer treatment options, expecting a total cure is not realistic. The fight is all about control, not elimination.
| Cancer Type | Chance of Cure (Stage IV) |
|---|---|
| Pancreatic | Less than 5% |
| Glioblastoma | About 5% |
| Metastatic Lung | Less than 10% |
Not great odds, but understanding this can help people make smarter choices about treatment, care, and what’s truly important to them moving forward.
Uncurable Cancers—A Closer Look
Some cancers simply don’t play by the usual rules. Even with the best treatments around, there are types where doctors can’t get rid of the disease completely. Here’s what that really means on the ground.
One of the toughest is glioblastoma. This is the most aggressive kind of brain tumor. Doctors can remove as much of the tumor as possible and then hit it with radiation and chemo, but it almost always comes back. The average survival time, even with treatment, is about 15 months. Only a tiny group make it much longer than that.
Pancreatic cancer is another hard hitter. Around 80% of folks diagnosed find out only after it’s already spread to places like the liver or lungs. Surgery isn’t an option for most people. The five-year survival rate is still in the single digits—think 10% or lower.
Then there’s metastatic lung cancer. When lung cancer has spread to other parts of the body, it usually can’t be cured. People do live longer now with targeted treatments and immunotherapy, but these approaches control the disease—they don’t cure it. The five-year survival rate for advanced stages is only around 8%.
Here’s a quick look at some numbers for the big three incurable cancers:
| Cancer Type | Stage When Found | 5-Year Survival Rate |
|---|---|---|
| Glioblastoma | Any | ~7% |
| Pancreatic | Usually late | <10% |
| Metastatic Lung | Stage 4 | ~8% |
It’s not just these cancers, though. Sometimes, breast cancer, prostate cancer, or even melanoma can become incurable if they spread too far or develop resistance to treatment. When doctors use the word “incurable,” it often means they aim to keep you living as long and as well as possible, not to make the cancer disappear forever.
If you or someone you know is facing one of these uncurable cancer types, up-to-date treatment still matters. There are always new trials, different medication mixes, and new ways to boost quality of life. Knowledge is power—so get your info from real sources and don’t be shy about asking your care team the tough questions.
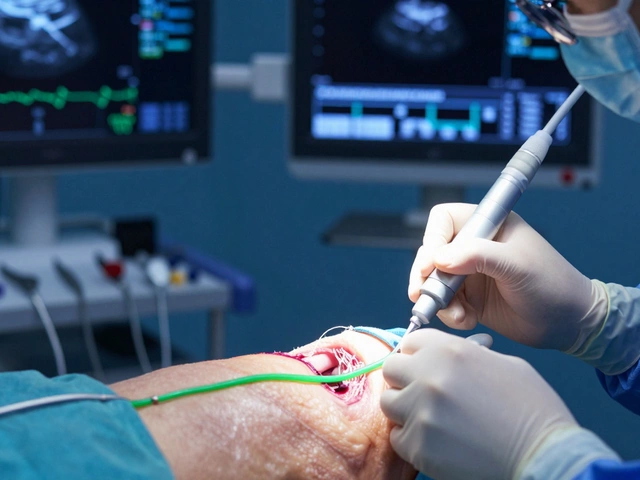
Modern Treatments: What’s Possible, What’s Not
When people hear that a cancer has no cure, it’s easy to think there’s nothing left to try. That’s far from the truth. Today’s cancer treatment menu has grown way beyond the old days of just chemo and radiation. Think immunotherapy, targeted drugs, and even gene therapy. But here’s the kicker—not all of these work for every cancer, and some cancers just find ways around them.
Let’s use incurable cancer as an example. For pancreatic and metastatic lung cancer, treatments usually focus on shrinking tumors, slowing them down, or making life more comfortable. In medical terms, it’s called “palliative care”—more about easing symptoms than promising a full-on cure. For some lucky cases, these treatments can push cancer into remission for a while, but doctors rarely talk about a clean bill of health.
Check out how some of the top treatments stack up for tough cancers:
| Treatment | Best For | Main Goal | Reality Check |
|---|---|---|---|
| Chemo & Radiation | Many advanced cancers | Shrink/slow tumors | Side effects, not always a cure |
| Immunotherapy | Melanoma, some lung cancers | Boost body’s own defenses | Helps some, not all |
| Targeted Therapy | Leukemia, breast, prostate | Attack certain cancer cells | Works if cancer has "the target" |
| Hormone Therapy | Breast, prostate | Block hormones that fuel cancer | Only for hormone-sensitive types |
| Palliative Care | All incurable cancers | Quality of life | No cure, but big quality boost |
One thing almost every oncologist agrees on: new drugs and combos do buy more good days. As Dr. Otis Brawley, former chief medical officer of the American Cancer Society, put it,
“We can sometimes turn cancer into a chronic disease that people live with for years, but in many cases, we can’t completely cure it.”
So, what’s possible? More time, better living, sometimes even long-term remission. What’s not? A guarantee that the cancer will never come back, especially if it’s already spread. The take-home is to ask tough questions about what any treatment can actually do for a specific case, and set real expectations. And remember, sometimes the focus shifts from curing to living well for as long as possible—that can be the real win.

Living with an Incurable Diagnosis
Getting told you have an uncurable cancer flips your world upside down. It’s normal to feel shock, anger, fear, and frustration—all mixed together. So what do you actually do next?
First, it helps to know that 'no cure' doesn’t mean doctors give up on you. Treatments can often keep cancer in check for months or even years. Many people with metastatic cancer live far longer than they first thought possible, thanks to modern treatments. The focus shifts from trying to "cure" the disease to controlling symptoms, slowing it down, and keeping you living as fully as possible.
Here are some real-world steps that help keep things manageable:
- Ask your doctor what you can expect day-to-day. Sometimes, simple changes—like tweaking medication or trying physical therapy—can make a big difference in your quality of life.
- Don’t be afraid to get a second opinion. With so many new treatments coming out, another oncologist might have a fresh idea.
- Palliative care isn’t about 'giving up'—it’s about tackling pain, stress, and side effects. People often start palliative care early now, right alongside cancer treatment.
- Stay connected with friends, family, or support groups. Talking through stuff helps, whether it’s a rough day or news about a new clinical trial.
- It’s smart to get your paperwork in order, too. Set up your medical wishes and talk honestly with your circle about what you want, even if it’s uncomfortable. It gives you some control back.
Here’s something you may not hear enough: studies show people who get good symptom management along with regular cancer treatment often live longer and feel better than those who only focus on the disease itself.
| Factor | Without Palliative Support | With Palliative Support |
|---|---|---|
| Average survival for metastatic lung cancer* | 8 months | 11.6 months |
| Reported quality of life | Low to moderate | Moderate to high |
*Data from New England Journal of Medicine, 2010 (Temel et al.)
It’s not about counting days. It’s about making the most of every single one, with treatments and choices that fit your needs. With all the new research (and sometimes sheer stubbornness), people keep finding ways to write their own story through cancer.
Breakthroughs and Hope on the Horizon
If hearing "uncurable cancer" gets you thinking there's nothing left but waiting, think again. The cancer world moves fast—researchers are working around the clock, and new treatments keep popping up that actually make a big difference. Even in the past few years, some stuff that sounded like science fiction is now on the table.
The first big game-changer: immunotherapy. Instead of blasting cancer with chemo, immunotherapy gets your own immune system to attack cancer cells. Checkpoint inhibitors, like pembrolizumab or nivolumab, have helped people with tough-to-treat cancers—think melanoma or some lung cancers—live way longer than expected before these drugs existed. They don't cure everything, but when they work, people can see years of extra life.
There's also targeted therapy. The idea is simple: find exactly what's making the cancer cells grow, then block that. This isn’t about treating everyone the same—doctors test your tumor for specific genes or proteins, then match you with a drug that targets your cancer’s weak spot. HER2-positive breast cancer is a good example—drugs like trastuzumab have changed the game.
Now, if you like numbers, check this out:
| Breakthrough | Year Approved (USA) | Cancer Types Impacted |
|---|---|---|
| Immunotherapy (Keytruda) | 2014 | Melanoma, lung, more |
| Targeted therapy (Trastuzumab) | 1998 | HER2+ breast, gastric |
| CAR T-cell therapy | 2017 | Leukemia, lymphoma |
Some terminal cancer types, like certain leukemias, now see kids and adults living for years—sometimes with no obvious cancer left after CAR T-cell therapy. Sure, not everyone gets that lucky, but it’s miles from where we were 20 years ago.
Researchers haven’t given up on tough cancers like pancreatic, brain, or metastatic prostate cancer. Clinical trials are always running. Even if something isn’t a "cure" yet, new drugs and combos can shrink tumors, slow growth, and sometimes turn an "incurable" cancer into a chronic illness you can manage for many years.
The takeaway? The word "no cure" isn’t set in stone. Treatments keep getting smarter, and more people are living fuller lives for much longer—thanks to cutting-edge science and a stubborn refusal to quit when it comes to cancer treatment.
Tips for Patients and Families
Coping with an uncurable cancer diagnosis hits hard. But there are ways to find control, hope, and support on this tough road. Here’s what helps, straight from doctors, nurses, and real families who’ve walked the path.
- Get Clear on the Plan: Ask your oncologist what treatments are meant to do—are they aiming to slow the cancer, ease symptoms, or buy more time? Knowing the goals helps when making choices.
- Pain and Symptom Management Matters: Don’t tough it out. Palliative care teams are there, even early in the journey, to make life feel better. They help with pain, sleep, anxiety, and more—no need to wait until things get really tough.
- Small Wins Add Up: Celebrate finishing a treatment round, a good lab result, or even just having the energy for a laugh or family dinner. These moments boost everyone’s mood.
- Talk About What Matters: It can be uncomfortable, but honest talks get everyone on the same page. Discuss priorities—whether it’s more time at home, a special trip, or getting legal paperwork in order so everyone feels less stressed.
- Build a Crew: No one handles terminal cancer alone. Bring in friends or support groups, both in person and online. Groups like CancerCare offer free counseling and tons of resources.
- Stay Informed, But Don’t Overdo It: The internet is full of info—sometimes too much. Stick to trusted sites like the American Cancer Society or your doctor’s resources. Don’t chase miracle cures you read about in Facebook comments.
- Financial Stuff is Real—Tackle It Early: Treatments, meds, and time off work add up. Social workers and hospital financial counselors can help you figure out insurance, disability, drug assistance, and local programs to cut costs.
Here’s a look at one key issue: out-of-pocket costs for cancer treatment. Even if you have insurance, bills can add up fast. A recent survey found:
| Cost Type | Average Monthly Expense (US) |
|---|---|
| Prescription Drugs | $700 |
| Doctor Visits & Procedures | $400 |
| Transport & Lodging | $150 |
Don’t be shy about asking for help—financial and emotional support can make a real difference. And if you’re a family member, don’t forget to look after yourself too. Caregivers often burn out, so take turns, share the load, and give yourself breaks. You can’t help if you’re totally drained.